Purpose: To evaluate the results of 3 cases with persistent macular holes (MH) treated by 23-gauge vitrectomy, extension of internal limiting membrane peeling, a human amniotic membrane (hAM) plug insertion into the subretinal space through MH and expanding gas endotamponade.
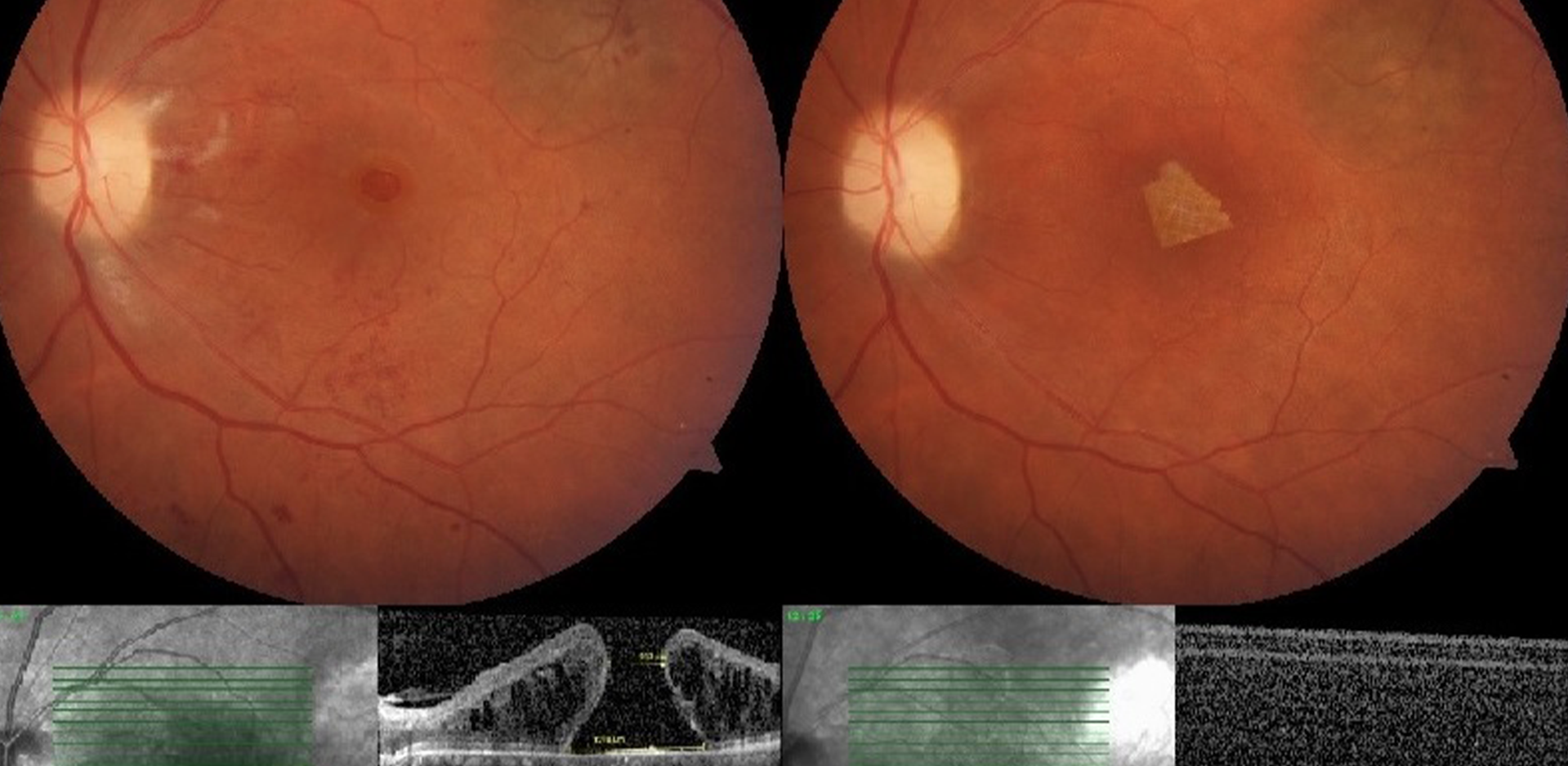
Material and methodology: The diagnosis of persistent MH in three patients was unilaterally confirmed using SD-OCT. In the first patient, a primary MH was present. In the second patient, a secondary MH occurred after cystoid macular edema because of central retinal vein occlusion. The third patient suffered with sustained atrophy of the retinal pigment epithelium (RPE) in the foveola several years before the development of MH. All patients were females. The first two patients underwent reoperation four months after the primary surgery; the third patient underwent two previous pars plana vitrectomies (PPVs), the last one 11 years ago. Firstly, a revision of the periphery and removal the vitreous remnants were performed; the ILM peeling zone was extended. The plug from the dehydrated hAM was prepared. Subsequently, the hAM plug was inserted via MH subretinally. Standard cryopexy behind the sclerotomies, fluid-for-air exchange, and vitreous cavity tamponade with expansile gas were performed.
Results: Two patients achieved MH closure; in the third patient, surgery significantly reduced cystoid edema of the MH edges and the MH diameter, but the MH remained open. All patients experienced a mild improvement in visual acuity and loss of disturbing visual phenomena.
Conclusion: We have confirmed that hAM plug insertion is feasible for persistent MH, even of large sizes. It is essential to orient the basal membrane of the plug towards the neurosensory part of the retina and the chorionic side to the RPE due to growth factors, but also for the concavity of the plug towards the RPE. It is possible that the use of tamponade with perfluoropropane (C3F8) is preferable to tamponade with sulfur hexafluoride (SF6). The time of reoperation approximately 3–4 months after the first failed vitrectomy can be considered optimal.